2025.12.09
What is Celiac Disease?
Celiac disease is an autoimmune disorder in which the body's immune system mistakenly attacks its own tissues. It primarily affects individuals who are genetically predisposed, carrying the DQ2 and DQ8 genes on chromosome 6. This disease occurs upon repeated exposure to gluten, a protein naturally found in wheat, barley, and rye. The term "gluten" is derived from the Latin word glue, referring to the way its two primary proteins, gliadin and glutenin, bind together to create a network that gives dough its elasticity and stickiness.
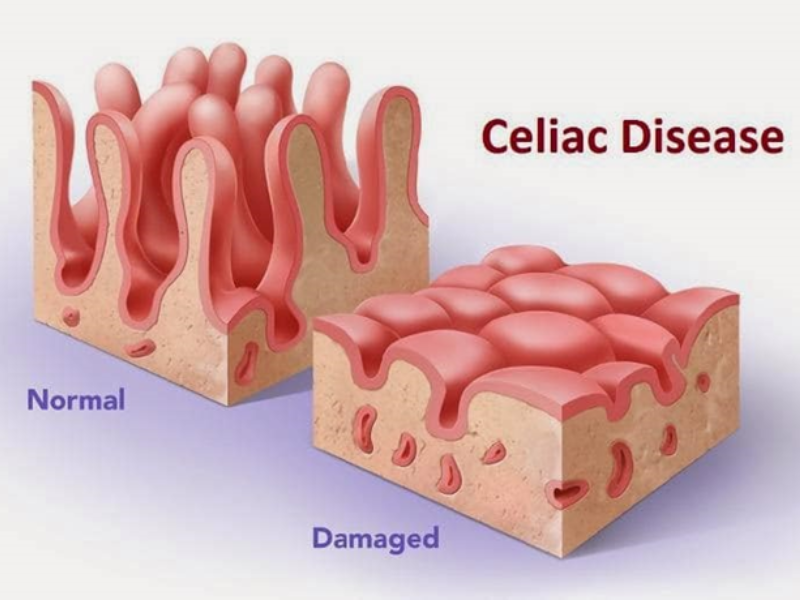
To better understand this disorder, it is helpful to compare the functioning of the small intestine in a healthy individual versus someone with celiac disease. In a healthy person, after food is swallowed through the mouth, it passes through the esophagus, is digested in the stomach, and reaches the small intestine. Nutrient absorption occurs in the small intestine with the help of small finger-like projections called villi, which are made of epithelial tissue. These villi increase the surface area of the intestinal wall, enhancing nutrient absorption.
In individuals with celiac disease, after consuming gluten-containing food and passing through the digestive tract into the small intestine, gluten is absorbed through the intestinal villi. However, due to the presence and expression of the DQ2 and DQ8 genes, certain proteins on the surface of immune cells recognize a fragment of gluten (mer-33 in alpha-gliadin) as a foreign invader. This recognition activates helper T lymphocytes, which stimulate other immune cells and produce antibodies (IgA and IgG). This leads to the production of killer T lymphocytes, whose main role is to attack cells infected with foreign agents.
In other words, killer T cells directly attack the cells of the small intestine. This immune response increases intestinal permeability, damages the intestinal cells, and causes the villi to deteriorate. Consequently, nutrient absorption and enzymatic activity in the intestine are reduced.
Causes of Celiac Disease
98% of celiac patients have the DQ2 and DQ8 genes, though this does not mean that everyone with these genes will develop celiac disease. In other words, the presence of these genes is necessary but not sufficient for the development of celiac disease.
Celiac disease is a multifactorial condition, meaning that besides the genetic predisposition provided by the DQ2 and DQ8 genes, the following factors also contribute to the onset of the disease:
Consumption of gluten-containing foods
Introducing gluten-containing complementary foods, such as wheat-based infant cereal (like wheat-based baby food), at an early age (for example, starting at four months old when breastfeeding is stopped) greatly increases the risk of developing celiac disease.
Research in 2024 has shown that bacterial infections in the digestive system with Escherichia coli and Shigella are associated with an increased risk of celiac disease. Changes in the gut microbiome—such as a reduction in beneficial bacteria like Bifidobacterium and Lactobacillus, and an increase in pathogenic bacteria like Escherichia coli and Staphylococcus—may play a role in the onset and severity of celiac disease. Beneficial gut bacteria can digest parts of gluten and reduce immune system activation. On the other hand, an increase in pathogenic bacteria may raise intestinal permeability and damage the intestinal lining, thereby linking microbial changes to celiac disease.
Improper use of antibiotics, as they act similarly to gluten by increasing the level of a protein called zonulin in the body, which leads to loosening the connections between intestinal cells and increased intestinal permeability, thus raising the risk of celiac disease, especially in children. It is important to note that avoiding unnecessary antibiotics—such as for viral illnesses—is advised. However, correct use of antibiotics for bacterial infections, as prescribed by a doctor, is essential.
Problems and Complications Caused by Celiac Disease
Some specialists refer to celiac disease as the "disease with a thousand faces" because the clinical signs of this condition are very diverse. In the past, only the gastrointestinal symptoms of the disease, such as bloating, abdominal pain, headaches, constipation, and chronic diarrhea, were considered. However, further studies have shown that in celiac disease, the destruction of the villi in the small intestine leads to reduced absorption of vitamins and nutrients. As a result, serious complications such as hair loss, anemia, iron deficiency, pregnancy disorders, behavioral disorders, irritability, seizures, vitamin D and calcium deficiencies, osteoporosis, fatigue, and memory disorders are observed.
Additionally, celiac disease can increase the risk of developing colon cancer and T-cell lymphoma (a type of cancer originating from a type of white blood cell called T-lymphocytes) because celiac disease causes excessive growth and division of immune cells (T-lymphocytes), which increases the risk of their transformation into cancerous cells.
In some cases, untreated individuals with celiac disease may also develop lactose intolerance or an intolerance to milk sugar. After consuming lactose-containing dairy products, they may experience stomach pain, diarrhea, etc. This occurs because damage to the intestinal cells reduces the ability to produce lactase, the enzyme responsible for breaking down lactose, which is produced by the cells of the small intestine wall. As a result, the individual cannot tolerate lactose in dairy products.
According to many studies, there is a strong connection between celiac disease and autoimmune endocrine diseases, such as type 1 diabetes and thyroid disorders. In other words, individuals with celiac disease are at a higher risk of developing diabetes and thyroid disorders. One reason for this is the overactive immune system in celiac disease, which mistakenly attacks the body’s own tissues and cells. This overactivity can damage the insulin-producing cells in the pancreas or the thyroid gland, leading to diabetes and thyroid problems. Another reason is that in celiac disease, the absorption of essential nutrients in the intestines, including amino acids required to produce pancreatic enzymes, is reduced, which impairs pancreatic function and increases the risk of diabetes. Additionally, nutrients such as selenium, which are essential for thyroid hormone production and activity, as well as magnesium, iron, vitamin D, and others that support thyroid function, are reduced in celiac disease, negatively affecting thyroid performance.
Celiac disease in mothers can lead to infertility and miscarriage. This is because, during attempts to conceive and during pregnancy, the absorption of essential vitamins and minerals, such as folic acid, vitamin B12, etc., is reduced in mothers with celiac disease due to the dysfunction of the small intestine. This impaired nutrient absorption leads to disrupted fetal growth and results in miscarriage in over half of pregnant women with celiac disease. Furthermore, because women with celiac disease typically have lower levels of estrogen—a hormone produced by fat tissues and other tissues—and often experience weight loss and reduced fat tissue, the lower estrogen levels can lead to infertility and menstrual cycle irregularities.
However, sometimes a person may have celiac disease without showing symptoms and may not realize they are affected. The onset of the disease can occur from childhood to old age, and nearly every organ, tissue, and system in the body can experience complications due to this disease.
Symptoms of Celiac Disease in Children
Once a child begins consuming gluten-containing foods, they often exhibit gastrointestinal symptoms such as diarrhea, abdominal pain, and vomiting. Other symptoms include inadequate growth and failure to gain weight. During school years, children may experience learning difficulties and academic decline, and during puberty, delayed puberty and short stature may occur.
History of Celiac Disease Diagnosis
Humans initially subsisted on meat, fruits, and vegetables without exposure to gluten-containing grains. About 10,000 years ago, in a region of the Middle East known as the Fertile Crescent—comprising parts of Iraq, Israel, Lebanon, Palestine, Syria, Kuwait, Turkey, and Iran—wild grains such as wheat and barley were cultivated due to favorable growing conditions. Over time, humans shifted from hunting and foraging for food to farming and animal domestication, marking the Neolithic Revolution. This shift from nomadic tribes to settled agricultural life allowed for food storage, and many people in this region migrated westward to obtain new lands for cultivation. After the introduction of grains into the human diet, many people's bodies adapted, but some did not, leading to the emergence of diseases like celiac.
Celiac disease may have ancient origins, with some evidence supporting this theory. For instance, in 2008, archaeological excavations in Italy led to the discovery of the remains of a woman, aged 18 to 20, from the 1st century AD, showing signs of stunted growth and malnutrition. Further analysis revealed the presence of celiac disease-related genes in this individual.
The Greek physician Aretaeus of Cappadocia, in the 2nd century AD, made the first known description of celiac disease, associating it with symptoms such as diarrhea and malabsorption. He used the term "coeliac" (from the Greek word koiliakos, derived from koilia, meaning belly).
In the 19th century, Dr. Samuel Gee, an English pediatrician, proposed a theory linking celiac disease to diet and suggested that dietary management could treat the disease. However, he could never determine the exact cause of celiac disease or which foods specifically triggered the condition. In some countries, September 13, Dr. Gee's birthday, is recognized as Celiac Awareness Day.
In 1924, Dr. Sidney Haas, an American pediatrician, treated children with celiac disease using a banana diet. Before this dietary intervention, over 30% of children with celiac disease died. The banana diet, which was unintentionally gluten-free and high in calories, helped these children improve their intestinal villi. Parents from across the United States sought Dr. Haas for treatment. However, by the early 1950s, the banana diet had limitations, as many parents mistakenly believed their children were "cured" and resumed a regular gluten-containing diet, which damaged the intestinal villi and caused a relapse.
In the 1940s, Dr. Willem Dicke, a Dutch pediatrician, proposed that a wheat-free diet was effective for treating celiac disease. He observed that during World War II, when bread was scarce in the Netherlands, the mortality rate from celiac disease decreased significantly, even reaching zero.
In 1925, a medical team shared their findings, showing that the removal of wheat and rye from the diet of individuals with celiac disease helped improve their condition. Later, gluten, the protein found in wheat, barley, and rye, was identified as the direct cause of celiac disease.
Prevalence of Celiac Disease
The prevalence of celiac disease in Iran, as in most countries, is around 1%. However, the prevalence varies across different provinces. According to the Center for Gluten Disorders, the disease is more common in provinces such as Ilam, Lorestan, Kurdistan, and Sistan and Baluchestan, where the prevalence exceeds 2%. In provinces like Fars, West Azerbaijan, and East Azerbaijan, the prevalence is less than 1%. The higher prevalence in certain regions has been attributed to factors such as gluten consumption and environmental factors, including gut microbiota.
The likelihood of developing celiac disease is higher in individuals with a family history of the disease, such as parents, siblings, or those with other autoimmune diseases, such as diabetes, thyroid disorders, and even Down syndrome. In families with a history of celiac disease, the probability of the disease occurring ranges from 3% to 22%. The prevalence of celiac disease in individuals with diabetes is around 6%, while in the general population, it is only 1%. Research in Iran has estimated the prevalence of celiac disease in diabetic patients to be between 3% and 8%. The prevalence of thyroid disease in individuals with celiac disease is four times higher than in the general population. Celiac disease is more common in women than in men, sometimes two to three times as frequent.
Initially, celiac disease was thought to affect only Caucasians of European descent. However, studies on regions such as Africa, the Middle East, Asia, and South America, which were previously thought to be free of the disease, revealed that celiac disease existed in these areas, but was undiagnosed.
As previously mentioned, individuals with the DQ2 and DQ8 genes are genetically predisposed to celiac disease. According to studies conducted on celiac patients, 85.7% of them had two copies of DQ2, 11.4% had two copies of DQ8, and 2.8% had one copy of either DQ2 or DQ8.
Celiac disease is a relatively common cause of chronic diarrhea in countries such as Iran, Iraq, and Kuwait, where wheat consumption is high.
Examining the Risk of Different Types of Wheat for Celiac Patients
One of the main culprits of celiac disease is a specific piece of gluten (mer-33 in alpha-gliadin), which is resistant to breaking down into its constituent amino acids in the digestive system and triggers the immune cells. This piece seems to exist on the D genome of wheat. Wheat genomes are diploid (AA), tetraploid (AABB), and hexaploid (AABBDD). Therefore, the likelihood of developing this disease is lower with the consumption of diploid and tetraploid wheat, which lack the D genome, compared to hexaploid wheat, which contains the D genome. As a result, tetraploid wheat (primarily durum wheat, used for pasta) and diploid wheat likely have less toxicity than bread wheat or hexaploid wheat for celiac patients. However, it should be noted that all types of wheat, even einkorn wheat, contain sequences that are dangerous for celiac patients.
Gluten-Containing Foods
Wheat, barley, rye, and foods containing these grains all contain gluten. However, some processed and packaged foods may have hidden gluten, meaning they may not list wheat, barley, or rye as ingredients, but could still contain gluten through additives, preservatives, and stabilizers like starch, maltodextrin, caramel coloring, malt, yeast, etc., which are derived from these grains. Additionally, some medications, dietary supplements, and even toothpaste or cosmetics may be made from derivatives of these grains and contain gluten.
Moreover, many times, even if a food product does not contain wheat, barley, rye, or their derivatives, it may still contain gluten due to cross-contamination. This occurs when a gluten-free food comes into contact with surfaces, utensils, or equipment that previously handled gluten-containing foods, thereby contaminating the food with gluten. For example, turmeric is inherently gluten-free, but if ground in a mill that previously processed gluten-containing products, it may become contaminated with gluten. Cross-contamination is so significant that products transported in bulk, such as foreign rice, can be contaminated with gluten. If the ship used to transport the rice previously carried wheat or barley, the contamination could be transferred to the rice, which is naturally gluten-free. It is even recommended for celiac patients not to place their utensils on a table, as they may be contaminated through cross-contact with gluten.
In some cases, starch is used to toast and salt nuts, so the salt sticks to them, or it may be used on dates to prevent them from sticking together. If the starch is derived from wheat, it will contain gluten. Some foods, like kebab or tomato paste, may not be suitable for celiac patients due to the potential addition of dry bread, and yogurt that contains stabilizers or starch should also be avoided, as the starch may be made from wheat.
The allowable gluten content in foods for celiac patients should not exceed 20 mg per kg.
Diagnosis of Celiac Disease
In suspected patients, a blood test is initially performed to measure specific celiac disease antibodies, including IgA and IgG antibodies against tissue transglutaminase (tTG) and IgA antibodies against endomysium (EMA). If these tests are positive, an endoscopy and biopsy of the small intestine are conducted to analyze the intestinal villi, definitively confirming the diagnosis of celiac disease.
Treatment of Celiac Disease
Currently, the only treatment for celiac disease is maintaining a lifelong gluten-free diet. This is because symptoms will return if the gluten-free diet is not followed after recovery. Due to the potential presence of gluten in some foods, it is recommended that celiac patients only consume products labeled as "gluten-free" or prepare foods such as yogurt, tomato paste, pickles, or toasting nuts at home to ensure they are not contaminated with gluten during processing.
In addition to avoiding gluten, patients may be advised to take vitamin, calcium, and iron supplements for several months after diagnosis to address any deficiencies in the body until the intestinal lining returns to normal and can absorb nutrients from food properly.